About Us
At Chronic Care Partner, we are more than just a chronic care company – we are your dedicated partner in managing and improving your health journey. Our mission is to provide comprehensive, personalized care solutions to enhance the well-being and quality of life for each of our patients. We take pride in our team of highly qualified clinical staff, all certified professionals based in the United States. Unlike many others, we do not outsource our services. This ensures that every aspect of your care is delivered with the highest standards and utmost dedication.
Chronic Care Management Model
The chronic care management model is an organizational approach to caring for people with chronic diseases in a primary care setting. Developed by Ed Wagner and his colleagues at the MacColl Institute for Healthcare Innovation in the late 1990s, the model aims to transform the daily care for patients with chronic illnesses from acute and reactive to proactive, planned, and population-based.
The Chronic Care Management Model typically encompasses several key elements designed to optimize care for patients with chronic conditions. Here are six essential elements of the Chronic Care Management Model:
2. Comprehensive Care Planning:
This element involves developing personalized care plans in collaboration with patients, caregivers, and multidisciplinary care teams. Care plans outline goals, treatment strategies, self-management support, medication management, and contingency plans for exacerbations or complications.
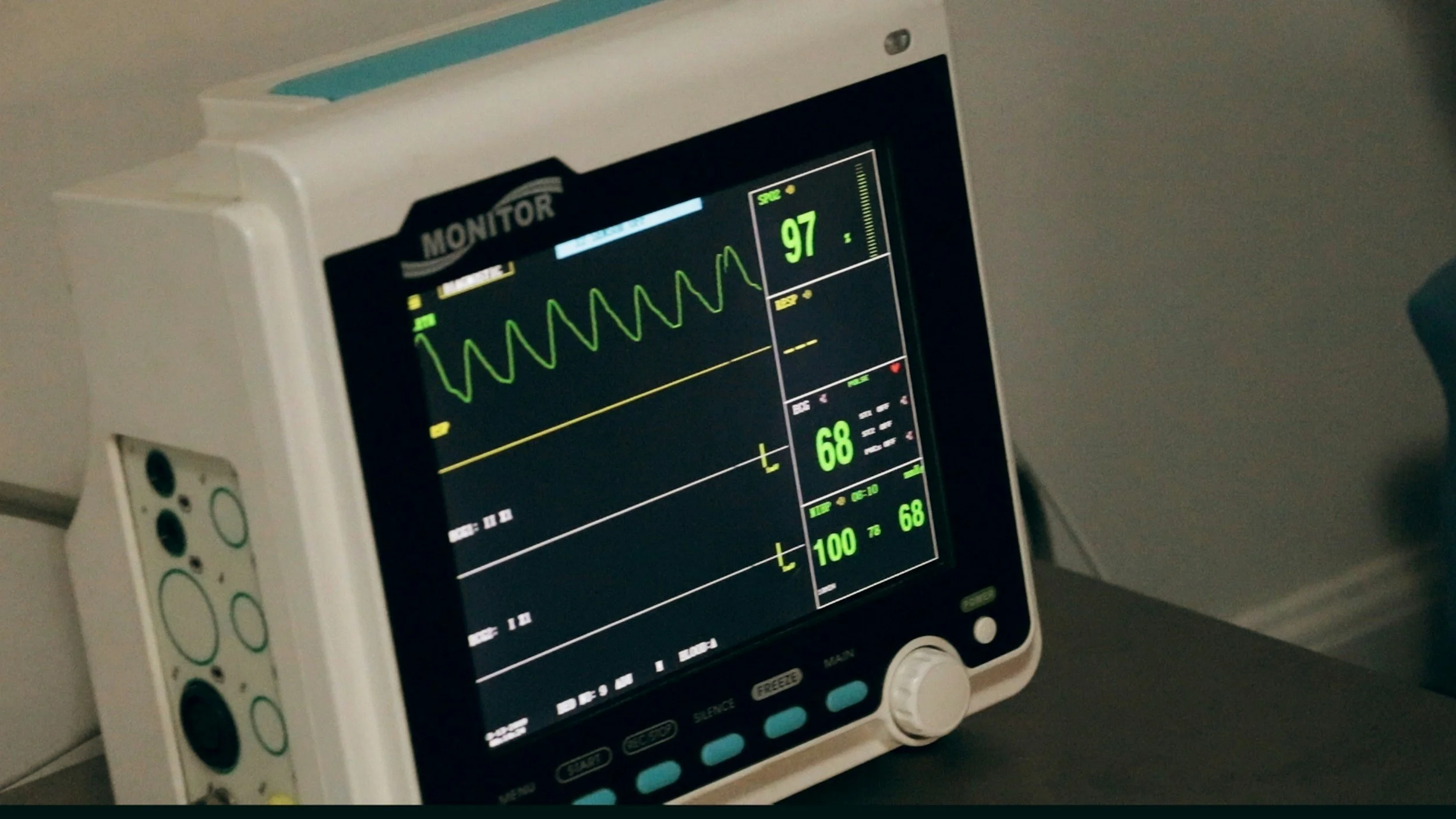
4. Proactive Monitoring and Follow-Up:
Regular monitoring and follow-up are critical for managing chronic conditions and preventing complications. This element includes tracking patient progress, conducting regular assessments, monitoring vital signs, lab results, and symptoms, and proactively addressing any changes or concerns.
6. Health Information Technology (HIT) and Data Integration:
Leveraging HIT and data integration tools facilitates efficient and effective chronic care management. This element includes using electronic health records (EHRs), patient portals, telehealth platforms, remote monitoring devices, and other technologies to streamline communication, documentation, and information sharing among care team members and patients.
1. Patient-Centered Care:
Within the Chronic Care Management Model, the focal point is on the needs, preferences, and objectives of the patient. It entails involving patients as active contributors to their care, promoting shared decision-making, and customizing interventions to suit individual circumstances and preferences.
3. Care Coordination:
Effective care coordination ensures seamless communication and collaboration among healthcare providers, specialists, community resources, and patients. It involves facilitating transitions of care, sharing information, and ensuring that patients receive appropriate services and support across different settings.
5. Self-Management Support:
Empowering patients to actively manage their health is essential for improving outcomes and quality of life. This element involves providing education, resources, and support to help patients develop self-management skills, adhere to treatment plans, make healthy lifestyle choices, and effectively manage their conditions at home.
Frequently Asked Questions
1. What is a chronic care management model, and how does it differ from traditional healthcare delivery?
A chronic care management model is a proactive approach to managing chronic conditions that focuses on continuous, coordinated care outside of face-to-face office visits. Unlike traditional healthcare delivery, which often emphasizes episodic care, chronic care management model prioritize ongoing support, education, and care coordination to improve patient outcomes and quality of life.
2. What are the key components of an effective chronic care management model?
Key components include comprehensive care planning, regular patient monitoring and follow-up, medication management, patient education and self-management support, care coordination with other providers, and leveraging technology to enhance communication and engagement.
3. How can adopting a chronic care management model benefit my patients?
Adopting a chronic care management model can benefit patients by providing personalized care plans tailored to their unique needs, improving medication adherence and self-management skills, reducing the risk of complications and hospitalizations, and enhancing overall quality of life through proactive management of chronic conditions.
4. What role do healthcare providers play in a chronic care management model?
Healthcare providers in a chronic care management model serve as care coordinators, educators, and advocates for their patients. They work collaboratively with patients to develop care plans, monitor progress, address barriers to care, and facilitate access to necessary services and resources.
5. How does a chronic care management model address the challenges of caring for patients with multiple chronic conditions?
A chronic care management model recognizes the complexity of managing multiple chronic conditions and prioritizes holistic, patient-centered care. By integrating services across different specialties, coordinating care transitions, and promoting self-management strategies, it helps optimize outcomes for patients with complex medical needs.
6. What are the financial implications of implementing a chronic care management model for my practice?
While there may be upfront costs associated with implementing a chronic care management model, such as staff training and technology investments, practices can realize long-term financial benefits through increased reimbursement for CCM services, improved patient retention and satisfaction, and reduced healthcare utilization.
7. How can technology and digital health tools support a chronic care management model?
Technology plays a crucial role in supporting chronic care management model by facilitating remote monitoring, telehealth visits, secure communication between patients and providers, electronic care plan documentation, and data analytics to track patient progress and outcomes.
8. What are some best practices for implementing a chronic care management model in my practice?
Best practices include engaging staff and patients in the change process, conducting comprehensive assessments of patient needs and practice workflows, providing ongoing training and support, fostering collaboration with community resources, and continuously evaluating and adjusting the model based on feedback and outcomes.
9. How can I ensure that my practice remains compliant with regulatory requirements when implementing a chronic care management model?
It’s essential to stay informed about regulatory requirements, such as those set forth by Medicare for billing CCM services, and ensure that your practice’s policies and procedures align with these guidelines. Regular audits and documentation reviews can help ensure compliance and mitigate risk.
10. Where can I find additional resources and support for implementing a chronic care management model in my practice?
Additional resources and support may be available through professional organizations, healthcare associations, academic institutions, and consulting firms specializing in chronic care management and practice transformation. Collaboration with peers and participation in learning collaboratives or quality improvement initiatives can also be valuable sources of support and guidance.